
Health Beliefs and Emotions Concerning Partners in Predicting HPV Vaccine Acceptability: Application of the Extended Health Belief Model
Abstract
This study applies an extended health belief model (HBM) to the intention to obtain a human papillomavirus (HPV) vaccination. This model incorporates perceptions of and emotions toward sexual partners in predicting the HPV vaccination intention. Path analysis tested two models that included different outcome variables (an intention to receive the HPV vaccine and an intention to vaccinate children). Undergraduate students (N = 247) were recruited for an online survey that measured the variables in the model. Results indicate that partner susceptibility, partner benefits, and HPV vaccination efficacy influenced behavioral intentions to receive the HPV vaccine, and partner guilt was a significant mediator in predicting participants' own vaccination intention. Partner benefits and HPV vaccination efficacy significantly affected participants' behavioral intentions to vaccinate their potential children, and partner hope was a mediator in predicting their intentions to vaccinate children. This extended HBM provides a comprehensive way to predict vaccination intention by including perceptions of and emotions toward sexual partners.
초록
본 연구는 확장된 건강신념모델을 사람유두종 바이러스(HPV) 백신 이슈에 적용하였다. 이 모델은 성적 파트너에 관한 인식과 감정을 HPV 백신 접종 의도를 예측하는 데 결합하였다. 경로 분석을 통해 다른 결과변수(자신이 HPV 백신을 접종하려는 의도와 자녀들에게 HPV 백신을 맞히려는 의도)를 포함한 두 개의 모델을 검증하였다. 이 모델에 포함된 변수들을 측정하는 온라인 설문조사를 위해 대학생(N =274)이 모집되었다. 연구 결과를 통해 파트너 취약성, 파트너 이익, HPV 백신 접종 효능이 HPV 백신을 스스로 맞으려는 의도에 영향을 끼치는 것으로 나타났으며, 파트너 죄책감은 백신 접종 의도를 예측하는 데 유의미한 매개변수였다. 파트너 이익과 HPV 백신 효능은 자녀들에게 백신을 맞히려는 의도에 유의미하게 영향을 미치는 것으로 나타났으며, 파트너 희망은 자녀들과 관련한 의도를 예측하는 데 매개효과의 역할을 하였다. 확장된 건강 신념 모델은 성적 파트너에 대한 인식과 감정을 포함함으로써 백신 접종 의도의 종합적인 예측력을 보여주었다.
Keywords:
Extended Health Belief Model, HPV Vaccination, Behavioral Intentions, Emotions키워드:
확장된 건강 신념 모델, HPV 백신 접종, 행동 의도, 감정1. Introduction
Human papillomavirus (HPV) infection is common among sexually active individuals and poses serious public health concerns because it can lead to further health problems (Centers for Disease Control and Prevention, 2019). HPV types 16 and 18 can cause cervical cancer among women (Baseman & Koutsky, 2005; Bosch, Lorincz, Muñoz, Meijer, & Shah, 2002), and men can also suffer from HPV-related diseases (e.g., genital warts; Centers for Disease Control and Prevention, 2016). Therefore, vaccination against HPV is recommended for both women and men (Meites, Szilagyi, Chesson, Unger, Romero, & Markowitz, 2019).
The Advisory Committee on Immunization Practices (ACIP) recommends routine HPV vaccination at age 11 or 12 and catch-up vaccinations through age 26 for those not adequately vaccinated (Meites et al., 2019). Three types of HPV vaccines have effectively prevented the infection and spread of HPV types 16 and 18: 9-valent HPV vaccine (9vHPV), quadrivalent HPV vaccine (4vHPV), and bivalent HPV vaccine (2vHPV) (Centers for Disease Control and Prevention, 2010, 2020; Markowitz et al., 2007). Since 2017, only the 9-valent HPV vaccine (Gardasil 9, Merck and Co., Inc.) has been available in the United States (Centers for Disease Control and Prevention, 2020; H. Y. Lee, Lust, Vang, & Desai, 2018).
Statistics on recent HPV vaccinations in the United States suggest the importance of treating college students as a key target demographic. HPV vaccination rates among adolescents have not reached Healthy People 2030’s goal of 80% (Office of Disease Prevention and Health Promotion, n.d.). Although the optimal age for catch-up vaccination against HPV extends to 26 years, college students’ vaccination rates fall short of Healthy People 2030’s goals (Office of Disease Prevention and Health Promotion, n.d.). Indeed, before 2020, only 51.1% of adolescents aged 13 to 17 were up to date with the HPV vaccine series, and vaccination rates for undergraduates were below 55% (H. Y. Lee et al., 2018; Walker et al., 2019). More recently, a 2023 survey demonstrated that only 54.2% of college students (57.1% female and 46% male) completed the HPV vaccine series (American College Health Association, 2023). Moreover, overall vaccination rates had decreased during COVID-19 (Kahn et al., 2023). Considering that college-aged people are at the greatest risk of HPV infection, understanding their HPV vaccination behaviors is crucial for developing effective public health policies and communication strategies tailored to this population (Goldfarb & Comber, 2022; McLendon et al., 2021).
In addition to overcoming the low rates of HPV vaccination among college students, promoting HPV vaccination to this population could have long-lasting impacts on their decisions to vaccinate their children later in life (Wilson et al., 2016), which suggests the need to explicate it as an ultimate outcome. Grasping college students’ intention to vaccinate their children in the coming years may provide us insight into predicting parents’ decisions concerning their children’s vaccination (Wilson et al., 2016). Whether adolescents are vaccinated for HPV is likely to be decided by their parents (Rositch, Liu, Chao, Moran, & Beavis, 2022). Thus, parental decisions have influencing power on vaccination rates across society (Rositch et al., 2022). In this light, scholars suggest that college students’ intention to vaccinate their potential children is a significant indicator of the next generation’s public health outcomes (Wilson et al., 2016). To wit, as a unique outcome, college students’ intention to vaccinate their potential children indicates society’s capabilities to protect the next generation’s health (Wilson et al., 2016). Thus, identifying the factors that influence future parents’ intentions to vaccinate their children can provide insights into developing strategies to increase HPV vaccination rates over generations.
This study aims to obtain insights for current and future generations by examining college students’ behavioral intentions (1) to receive the HPV vaccine themselves and (2) to vaccinate their children for HPV as outcome variables. To this end, the present study builds on the extended health belief model (HBM) to develop a theoretical model for identifying how individuals engage with HPV vaccination (Donadiki et al., 2014). Numerous studies have used the original HBM to predict preventive health behaviors, such as smoking cessation (Schofield, Kerr, & Tolson, 2007) and breast cancer screening (Wu et al., 2006). The HBM assumes that individuals will adopt a given health behavior when they consider themselves susceptible to a disease, its consequences will be serious for themselves, the health threat can be avoided through action, the benefits of executing the health behavior may outweigh its costs, and they believe that they are capable of performing the behavior (Janz & Becker, 1984; Rosenstock, 1974; Rosenstock et al., 1988). Accordingly, the HBM addresses beliefs about health threats to oneself only, not beliefs about others. Thus, the HBM for oneself may not be applicable to the context of HPV infection, which is sexually transmitted (Centers for Disease Control and Prevention, 2016; Fallucca et al., 2022). Including additional factors in the model to reflect the nature of infectious diseases will enhance the original HBM’s contextual applicability. In the context of HPV vaccination, despite the empirical evidence explaining vaccination decisions, the model cannot fully account for treating HPV infection as a shared responsibility between sexual partners (Centers for Disease Control and Prevention, 2019). Thus, expanding the HBM requires consideration of sexual partners’ needs and health beliefs.
Furthermore, the conventional HBM includes only cognitive factors (i.e., health beliefs) and does not include emotions as predictors of health behavior. Scholars have criticized its omission of affective aspects from health behavioral research and proposed including affective factors in predicting health behaviors (Bagozzi & Moore, 1994; Wang, 2023). This proposed expansion of the model to include emotional aspects may enhance the effectiveness of the HBM in predicting health behaviors and guiding constructive public health interventions (Xiao, Lee, Wong, & Borah, 2021).
To address the theoretical gaps in the context of HPV transmission, this study proposes and tests an extended HBM model that includes health beliefs about and emotions toward sexual partners.
2. Literature Review
1) Health Belief Model
The HBM provides a useful theoretical framework for understanding college students’ HPV vaccination decisions (Donadiki et al., 2014; Fallucca et al., 2022; Oh, Alqahtani, Chang, & Cox, 2023). Indeed, as cognitive factors and beliefs determine preventive behaviors, cognitive models were effective for predicting HPV vaccination behaviors (Fallucca et al., 2022). The HBM has been widely used as a cognition-based theoretical framework (Fallucca et al., 2022). The HBM delineates the belief-based antecedents of health behaviors: perceived severity (assessment of how serious a health threat and its consequences are), perceived susceptibility (assessment of how vulnerable one is to a health condition), perceived benefits (assessment of whether the recommended action will reduce the health threat), perceived barriers (assessment about the difficulties or negative consequences of executing the recommended action), and self-efficacy (assessment of one’s ability to take action) (Austin et al., 2002; Montanaro & Bryan, 2014). The model assumes that health beliefs predict intentions to perform specific health behaviors (Rosenstock, 1974). The HBM can explain acceptance of specific health behaviors, including condom use (Macintyre et al., 2004; Zak-Place & Stern, 2004), breast cancer screening (Janz & Becker, 1984; Wu et al., 2006), smoking cessation (Schofield et al., 2007), and exercise (Fallon, Wilcox, & Ainsworth, 2005; Schwarzer et al., 2007). More germane to this study, a systematic review revealed that most HBM constructs are significantly associated with HPV vaccine acceptability, including behavioral intentions or willingness to perform specific health behaviors (Alsulami et al., 2023; Brewer & Fazekas, 2007). Although HBM constructs have been found to predict health preventive behaviors, earlier reviews of HBM research have found that effect sizes vary across the model’s constructs, suggesting that a novel approach could yield greater predictive power (Carpenter, 2010; Harrison et al., 1992; Xiao et al., 2021).
2) Extended Health Belief Model: Perceptions of Partners
This study extends the HBM to the context of HPV vaccination. The original HBM focuses on beliefs about health threats and preventive behavior, which are related only to oneself. The extended HBM expands this scope by incorporating individuals’ perceptions of their sexual partners in the context of HPV transmission. HPV is a sexually transmitted infection (STI), and sexual partners are naturally considered to be responsible for HPV transmission (Centers for Disease Control and Prevention, 2019; Staggers et al., 2012). Indeed, in a qualitative study investigating men’s perceptions of the HPV vaccine, focus group participants reported their sense of responsibility for their sexual partners’ HPV infections (Staggers et al., 2012). Perceived responsibility has been investigated as a variable of interest for health communication (Steins & Weiner, 1999). Research has demonstrated that perceived responsibility leads to pity and anger, where pity is associated with helping behaviors (Steins & Weiner, 1999). Another qualitative study indicated that HIV-seropositive male participants reported a sense of personal responsibility for protecting their partners from HIV infection, which suggests that perceived responsibility may be a key factor driving acceptance of risk-reducing actions (Wolitski et al., 2003).
The reviewed literature on perceived responsibility indicates that caring about the health of sexual partners should be considered a predictor of HPV vaccination. In this sense, clarifying how perceptions of one’s sexual partners predicts one’s own HPV vaccination, the extended HBM explicates perceptions of partners’ susceptibility to the disease and its severity for them, as well as the perceived benefits to one’s partner from undertaking preventive behavior. Previous research has also shown that extending the model in this direction is feasible. One study found that the altruistic motive of protecting female health was a significant predictor of HPV vaccine acceptance among male survey participants (Bonafide & Vanable, 2015). Another study that explored young men’s health beliefs found that perceived HPV infection susceptibility and severity for oneself and one’s female partner are both related to intentions to reduce the number of sexual partners (McPartland et al., 2005). Despite its importance and applicability in HPV-related contexts, the HBM has not yet been extended to include consideration of sexual partners. Thus, the present study contributes to the literature by proposing an expanded model that includes consideration of sexual partners to predict individuals’ HPV vaccination intention.
Consideration of sexual partners may be extended to vaccination decisions regarding one’s future children. According to previous studies, parents who vaccinated their children for HPV reported that the perceived benefit of protecting their children’s future sexual partners influenced their decision (Radisic, Chapman, Flight, & Wilson, 2017; Schuler, DeSousa, & Coyne-Beasley, 2014). This finding suggests that college students’ consideration of their sexual partners may also predict their intentions to vaccinate their potential children. This consideration may denote their viewpoint as future parents that HPV infection may be critical for partners. Thus, unmarried college students’ vaccination intention for their potential children could be predicted by their consideration of sexual partners, which is tested as a portion of the extended HBM.
3) Extended Health Belief Model: Emotions
Scholars have found that including only cognitive factors in the model is inappropriate for predicting behavior, as emotional factors can be influential (Bagozzi & Moore, 1994; Wang, 2023). To address the gap in the previous literature and increase the predictive power of the HBM, this study explores the role of guilt and hope as mediators between health beliefs and HPV vaccination intentions. Among the discrete emotions, these two emotions were known as predictors of diverse health behaviors, suggesting their potential effects on the behaviors of our interest (Ellsworth & Smith, 1988; Izard, 1977; Smith, Haynes, Lazarus, & Pope, 1993).
Guilt is usually accompanied by remorse and a sense of responsibility, thus encouraging the adherence to a recommended course of action with the goal of reducing guilt (Izard, 1977). Previous studies have found that feeling guilty is associated with a range of health behaviors, such as decreased alcohol and drug use (Dearing et al., 2005), increased condom use (Wayment & Aronson, 2002), and increased physical activity (Eyler & Vest, 2002). Similarly, hope, a forward-looking emotion, is driven by positive prospects of future outcomes (Ellsworth & Smith, 1988; Smith et al., 1993). Indeed, hope prompts individuals to perform behaviors that may help them achieve their goals (Averill et al., 1990). For instance, scholars have demonstrated that feelings of hope are related to cervical cancer screening intentions (Kim & Hmielowski, 2017) and sun safety behavioral intentions (Nabi & Myrick, 2019). Few empirical studies have employed the HBM to examine the role of hope and guilt in health decisions (Wang, 2023). Wang (2023) found that guilt mediated the direct effect of perceived susceptibility to COVID-19 on the intention to receive the COVID-19 vaccine, and hope mediated the direct influence of perceived benefits on the vaccination intention.
Accordingly, this study extends the HBM by adopting perceptions of partners (susceptibility, severity, and benefits), guilt about partners’ HPV infection, and hope of preventing partners’ HPV infection among the model variables. Overall, this study investigates (1) how the newly added variables affect one’s own HPV vaccination intentions and behavioral intentions to vaccinate one’s children and (2) whether partner-oriented emotions (i.e., guilt and hope) mediate the relationship between health beliefs and behavioral outcomes.
3. Method
1) Sample
Undergraduate students at two large universities in the United States participated in an online survey for course credit in summer 2015 (June 18 to July 7, 2015) and fall 2015 (October 26 to December 4, 2015). A total of 668 individuals completed the questionnaire, all of whom were 18 or older and heterosexual. Only respondents who indicated that they had not received the HPV vaccine were included, resulting in 247 cases for data analysis. Table 1 reports detailed sample characteristics.
2) Measures
The study variables can be categorized into three groups: “antecedent” endogenous variables (those influenced by some variables in the model and also influencing other variables), the “consequent” endogenous variables of interest, and exogenous variables (those not influenced by other variables in the model). Unless indicated otherwise, responses were recorded on a 7-point scale anchored at “strongly disagree” (1) and “strongly agree” (7).
Seven variables served as antecedent endogenous variables. Partner susceptibility was assessed using two items adapted from existing studies (Gerend & Barley, 2009; Gerend & Shepherd, 2012). Partner susceptibility addressed perceptions of partners’ susceptibility to infection (e.g., “If you do not get vaccinated for HPV, how likely do you think it is that your partner(s) will become infected with HPV in the future?”; r = .85, p < .001; M = 3.07, SD = 1.43). Partner severity was assessed with four items adapted from an established scale (Gerend et al., 2008). This scale addressed the negative consequences of HPV infection for participants’ partners (e.g., “If my partner(s) were infected with HPV, it would be disruptive to their physical health”; Cronbach’s α = .91, M = 5.19, SD = 1.26). Partner benefits were assessed with a three-item scale (Gerend et al., 2008; Gerend & Barley, 2009). The partner benefits measure covered the perceived benefits of HPV vaccination for participants’ partners (e.g., “If I get vaccinated for HPV it may be a good thing to do for my partner(s)’ health”; Cronbach’s α = .95, M = 4.85, SD = 1.42). The measure of perceived barriers comprised six items derived from an existing scale (Fang et al., 2007) (e.g., “Having the HPV vaccine will be painful and unpleasant”; Cronbach’s α = .78, M = 3.57, SD = 1.04). The measure of HPV vaccination efficacy was derived from three items used in a previous study (Fang et al., 2007) (e.g., “I am confident about my ability to receive the HPV vaccine”; Cronbach’s α = .80, M = 4.47, SD = 1.25).
The measure of guilt toward one’s partner comprised four items (Boudewyns et al., 2013). They addressed whether respondents would feel guilty if their partners were infected with HPV (e.g., “I would feel guilty if I found out my partner(s) had HPV”; Cronbach’s α = .93, M = 4.67, SD = 1.58). Hope toward one’s partner was assessed using five items that captured how hopeful, confident, expectant, encouraged, and optimistic respondents felt about preventing their partners from being infected with HPV (Ellsworth & Smith, 1988). For this measure, responses were recorded on a 7-point scale ranging from “not at all” (1) to “extremely” (7) (Cronbach’s α = .94, M = 4.75, SD = 1.51).
Two variables served as our final outcomes. First, participants’ behavioral intentions to receive the HPV vaccine were assessed with four items utilizing a 7-point response scale of “very unlikely” (1) to "very likely" (7) (e.g., “How likely is it that you will try to receive the HPV vaccine?”) (Gerend et al., 2008; Gerend & Shepherd, 2007). This measure addressed the extent to which participants viewed receiving the HPV vaccine themselves as acceptable (Cronbach’s α = .97, M = 4.20, SD = 1.65). Second, behavioral intentions to vaccinate one’s children for HPV were measured with four items (e.g., “How likely is it that you will try to have your children receive the HPV vaccine?”) (Gerend et al., 2008; Gerend & Shepherd, 2007) utilizing a 7-point response scale ranging from “very unlikely” (1) to “very likely” (7) (Cronbach’s α = .98, M = 4.49, SD = 1.60).
Exogenous variables included age, gender, race/ethnicity, prior STD testing, existence of current sexual partner, health efficacy, HPV knowledge, and timepoint of taking the survey (i.e., summer 2015 or fall 2015). Health efficacy was measured with a four-item scale (S. Y. Lee et al., 2008) (Cronbach’s α = .91, M = 5.50, SD = 1.04). HPV knowledge was evaluated with 23 true/false questions, and the number of correct answers was counted to create a knowledge index (McPartland et al., 2005; Shand et al., 2010) (Cronbach’s α = .92, M = 9.77, SD = 5.33). The timepoint of taking the survey was recorded as a dichotomous variable; 85% took the survey during fall 2015. The purpose of including these variables was to control for their effects on the tested models.
3) Statistical Analyses
To test the overall fit of the hypothesized mediation models, path analysis using structural equation modeling (SEM) was employed. SEM path analysis allows for estimation of direct and indirect effects as well as for testing all components of the mediation model simultaneously (Kline, 2011). We used the R package lavaan to test two separate models with different outcome variables: behavioral intentions to receive the HPV vaccine oneself and behavioral intentions to vaccinate one’s children. To control for variables that may affect the results, the residual values for all nine focal variables were obtained through regression using SPSS version 27. These residuals signified variances not explained by the covariates (Kline, 2011). Then, we used these residual values and fit a saturated model with all possible structural paths freed to be estimated. Second, all nonsignificant paths between independent variables and each of the two final outcome variables were removed to more closely examine the significant mediation effects, resulting in two final models (Kline, 2011).
3. Results
As shown in Figures 1 and 2, the two models fit the data well. The chi-square value was 7.69 (5, n = 247) for the first model (Figure 1), predicting behavioral intentions to receive the HPV vaccine (p = .17, comparative fit index [CFI] = .99, normed fit index [NFI] = .98, root mean square error of approximation [RMSEA] = .05). The first model explained 48.8% of the variance in behavioral intentions to receive the HPV vaccine. For the second model (Figure 2) predicting behavioral intentions to vaccinate one’s children for HPV, the chi-square value (6, n = 247) was 7.25 (p = .30, CFI = 1.00, NFI = .98, RMSEA = .03). The second model predicted 45.3% of the variance in behavioral intentions to vaccinate one’s children for HPV.
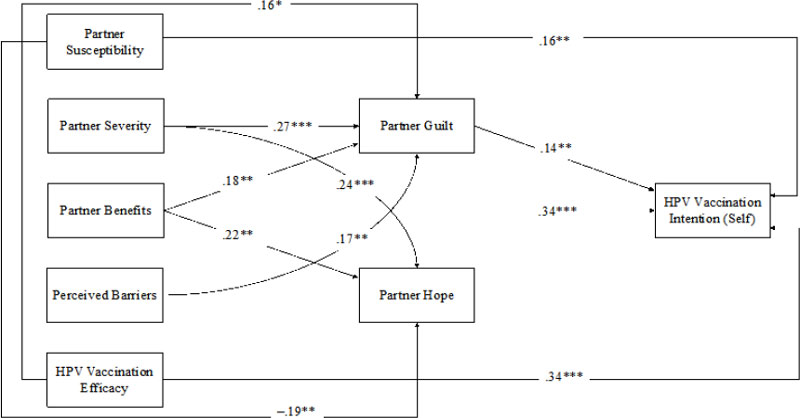
Model Predicting Behavioral Intentions to Receive HPV VaccineNote. Coefficients are standardized regression coefficients.*p < .05. **p < .01. ***p < .001.
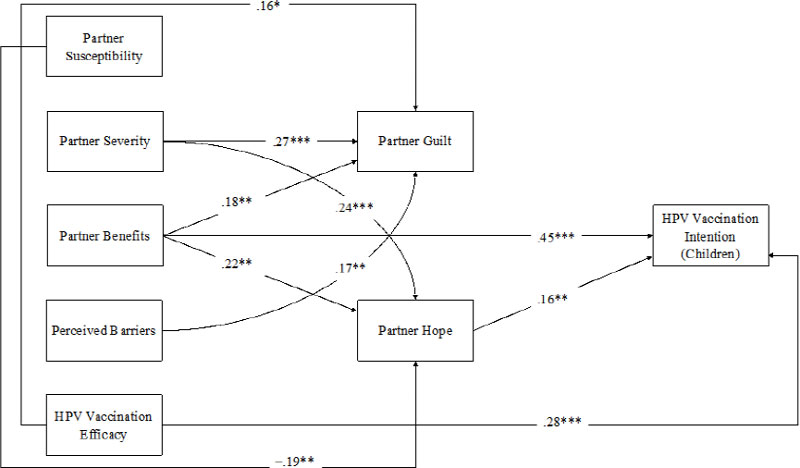
Model Predicting Behavioral Intentions to Vaccinate One’s Children for HPVNote. Coefficients are standardized regression coefficients.*p < .05. **p < .01. ***p < .001.
1) Effects on Behavioral Intentions to Receive HPV Vaccine
As Figure 1 demonstrates, partner susceptibility (β = .16, p < .01), partner benefits (β = .34, p < .001), and HPV vaccination efficacy (β = .34, p < .001) had direct effects on behavioral intentions to receive the HPV vaccine. These results suggest that the more that individuals perceive that their partners are susceptible to HPV infection, the more that their HPV vaccination would benefit their partners, and the greater their perceived capability of receiving the vaccine, the more they intend to vaccinate themselves against HPV. The direct effects of health beliefs on the behavioral outcome were supplemented by exploring indirect effects through partner guilt. The results indicated that partner severity (b = .04, Z = 2.44, p < .05), partner benefits (b = .03, Z = 2.01, p < .05), and perceived barriers (b = .33, Z = 2.03, p < .05) had positive indirect relationships with behavioral intentions to receive the HPV vaccine through partner guilt. Partner severity (β = .27, p < .001), partner benefits (β = .18, < .01), and perceived barriers (β = .17, p < .01) were positively related to partner guilt, which then influenced behavioral intentions (β = .14, p < .01). Unlike these significant indirect effects, the indirect effect of HPV vaccination efficacy on the outcome variable through partner guilt was not significant (b = .03, Z = 1.87, p = ns).
2) Effects on Behavioral Intentions to Vaccinate One’s Children for HPV
As Figure 2 shows, partner benefits (β = .45, p < .01) and HPV vaccination efficacy (β = .28, p < .01) have direct influences on behavioral intentions to vaccinate one’s children for HPV. This finding showed that individuals who perceived that their HPV vaccination would benefit their partners and that they were capable of receiving the vaccine were likely to have stronger intentions to vaccinate their children. The mediator of partner hope explained the direct relationship between health beliefs and behavioral intentions. Partner susceptibility had a negative indirect effect on behavioral intentions to vaccinate children against HPV through partner hope (b = -.28, Z = -2.17, p < .05). On the other hand, partner severity (b = .04, Z = 2.48, p < .05) and partner benefits (b = .04, Z = 2.29, p < .05) had positive indirect effects. Further, partner susceptibility (β = -.19, p < .01) was negatively associated with partner hope, but partner severity (β = .24, p < .001) and partner benefits (β = .22, p < .01) were positively associated. Lastly, partner hope had a positive relationship with intentions to vaccinate children (β = .16, p < .01).
4. Discussion
1) Key Findings and Implications
This study provides empirical support for the extended HBM, demonstrating the model’s ability to predict college students’ behavioral intentions to (1) receive the HPV vaccine and (2) vaccinate one’s children against HPV. Specifically, observing participants’ perceptions of others (namely, sexual partners) explained their own health behaviors. In addition, emotions toward a partner’s HPV infection (i.e., partner guilt) and toward prevention of a partner’s infection (i.e., partner hope) were explained by health beliefs and were significant predictors for HPV vaccination intentions.
This study has several theoretical implications. First, the health beliefs and emotions regarding one’s partner were tested to extend the original HBM. Indeed, although HPV infection cannot be explained without partner influence, prior studies have focused on how individuals’ health beliefs about themselves determine their own health behaviors (Donadiki et al., 2014). Given this missing link, the present study suggests a novel approach to increase the predictive power of the HBM and provides a theoretical account of how to encourage people to vaccinate themselves against HPV.
In addition, by including guilt and hope, this study developed a more comprehensive cognitive-affective model, providing greater ecological validity. This study contributes to theory building in terms of addressing HPV vaccination intentions with the serial influences of cognitive and affective factors. In this sense, emotions help discern the mechanism underlying the relationship between health beliefs and behaviors. However, partner hope was not a significant mediating variable in predicting behavioral intentions to receive the HPV vaccine, and partner guilt was not a mediator in the model predicting behavioral intentions to vaccinate one’s potential children. These findings indicate that different emotions guide individuals toward different behaviors. Guilt and hope are characterized by different core relational themes (Smith & Lazarus, 1993). The relational theme of guilt is self-blame, which reflects accountability applied to oneself (Smith et al., 1993; Smith & Lazarus, 1993). Considering that guilt was measured regarding partners’ possible HPV infection, the feeling of guilt is likely to promote perceived responsibility for partners’ health status, which may determine their intentions to receive the HPV vaccine. On the other hand, hope’s relational theme is effortful optimism, which can be explained by positive expectations for success (Smith et al., 1993). In this sense, hope of preventing partners from being infected with HPV seems to relate to positive future outcomes. By nature, hope seemingly motivates intentions to vaccinate potential children, given that the time orientation for hope and the behavioral intentions of individuals as potential parents is the future (Ellsworth & Smith, 1988; Smith et al., 1993). The mediation results demonstrated that different mechanisms generated different outcomes. Future research should explore the role of emotions in influencing individuals to engage in various health behaviors.
This study individually investigated college students’ intentions to vaccinate themselves and intentions to vaccinate their potential children. Predicting health behaviors at different times and targets provides a more holistic understanding of how particular health behaviors are determined. Particularly, the intentions of future parents in the U.S. to vaccinate their children indicate how well the health of the next generation will be protected (Wilson et al., 2016) while also providing insight into the current and possible future states of HPV vaccination. On a theoretical note, this study found that college students’ consideration of sexual partners extended its effects on the intention to vaccinate their future children. This result may indicate that college students’ consideration of sexual partners serves as a general factor in generating perceptions of HPV infection’s adverse effects on sexual partners. This finding aligns with previous research showing that parents tend to consider their children’s future sexual partners when making parental vaccination decisions (Radisic et al., 2017; Schuler et al., 2014). Future research needs to further explicate how beliefs about one’s partner affect the intention to vaccinate potential children.
This study also suggests important practical lessons for developing public health campaigns focusing on HPV vaccination among college students. On the one hand, it is important for health communication practitioners to remember the role of individuals’ consideration of their partners’ well-being in encouraging HPV vaccination. On the other hand, practitioners should understand that different emotions can generate different behaviors. These key takeaways may apply to designing messaging about other health topics. For example, regarding secondhand smoking, conveying altruistic motives toward others in messaging may enhance public health campaigns’ effectiveness (Borgstede et al., 2014).
This study also provides insights about audience segmentation in health campaigns. When designing a health campaign, it is important to identify the characteristics of target message recipients and to tailor message features accordingly (Chon & Park, 2017). Indeed, audience segmentation is an effective tool for delivering health messages to a specific group of people and leveraging strategic initiatives to influence their health behaviors (Chon & Park, 2017). Using the variables from the extended HBM for audience segmentation could guide communication practitioners in considering different foci for targeting each segment. For example, this study’s findings suggest that practitioners should strategically maneuver their communicative efforts to target college students with low levels of threat beliefs (i.e., partner susceptibility and partner severity).
2) Limitations and Future Directions
This study has a few limitations that can lead to future research directions. First, we recruited a convenience sample of undergraduate students from two U.S. universities, which may not adequately represent all U.S. college students. Future research should recruit a more diverse and representative sample to ensure our findings’ generalizability. Second, this study tested the extended HBM model in the context of HPV vaccination. To further validate the proposed extended HBM and understand its boundary conditions, more empirical testing of the theory would be needed in different disease contexts. Immunization and infectious diseases (including COVID-19), viral hepatitis, influenza, and tuberculosis are all feasible alternatives to explore. By integrating perceptions of others’ susceptibility to a disease and its severity for them as well as the perceived benefits for others of undertaking preventive behavior, future research should define the limits of the proposed model’s generalizability. Third, this study could not assess actual vaccination decisions that participants intended to make as parents in the future. Prediction of college students’ intentions to vaccinate their potential children may be limited if the assumptions that they will actually have children and they have the plan to get married anot satisfied. Even so, considering college students as future parents and exploring their intentions to vaccinate their potential children against HPV is critical for future-parent education, as parental support is an essential determinant of childhood vaccination (Wilson et al., 2016). In this regard, future research may increase predictive validity regarding parents’ vaccination decisions by recruiting current parents. Additionally, considering that HPV vaccination is recommended for adolescents ages 11 to 12, (Centers for Disease Control and Prevention, 2019) participants in this study were asked to indicate the likelihood of a vaccination decision in the distant future. It would be more appropriate for future studies to examine college students’ perceptions of other types of routine vaccines recommended for younger children (e.g., Hepatitis B; Measles, Mumps, and Rubella; and Chickenpox vaccines).
This study was conducted in 2015; thus, future studies must account for recent changes surrounding the HPV vaccine and replicate the findings of the current study. The 9-valent HPV vaccine became the only available vaccine in the U.S., and the ACIP stated shared decision making for those ages 27 through 45 (H. Y. Lee et al., 2018; Meites et al., 2019). Further investigation is needed to discern how these changes in HPV vaccination practices influence future vaccination behavior. Lastly, while this study focused on perceptual and emotional factors in relation to participants’ partners, future research might consider additional antecedents and outcomes. For instance, examining how other discrete emotions (e.g., pride, anger, and happiness) (Lazarus, 1991) and prior vaccination experiences affect vaccination decisions is an avenue for further investigation. Other vaccination related behaviors such as positive word-of-mouth about vaccination may also be examined as an outcome.
3) Conclusion
These research findings have theoretical and practical implications for public health promotion among college students. This study proposed a comprehensive model to predict individuals’ health behavioral intentions with respect to health beliefs and emotions in tandem with perceptions of their partners. The extended HBM adequately predicted vaccination intentions, indicating the necessity of incorporating additional variables in the model. The significant mediating role of emotions indicated a psychological process that results in greater vaccination intentions in the extended HBM. Taken together, this study suggests effective strategies for promoting public health in the context of HPV vaccination.
References
-
Alsulami, F. T., Sanchez, J., Rabionet, S. E., Popovici, I., & Baraka, M. A. (2023). Predictor of HPV vaccination uptake among foreign-born college students in the U.S.: An exploration of the role of acculturation and the health belief model. Vaccines, 11(2), Article 2. https://doi.org/10.3390/vaccines11020422
[https://doi.org/10.3390/vaccines11020422]

- American College Health Association. (2023). American College Health Association-national college health assessment III: Undergraduate student reference group executive summary spring 2023. https://www.acha.org/documents/ncha/NCHA-III_SPRING_2023_UNDERGRAD_REFERENCE_GROUP_EXECUTIVE_SUMMARY.pdf
-
Austin, L. T., Ahmad, F., McNally, M.-J., & Stewart, D. E. (2002). Breast and cervical cancer screening in Hispanic women: A literature review using the health belief model. Women’s Health Issues, 12(3), 122-128. https://doi.org/10.1016/S1049-3867(02)00132-9
[https://doi.org/10.1016/S1049-3867(02)00132-9]

-
Averill, J. R., Catlin, G., & Chon, K. K. (1990). Rules of hope. New York, NY: Springer-Verlag.
[https://doi.org/10.1007/978-1-4613-9674-1]

-
Bagozzi, R. P., & Moore, D. J. (1994). Public service advertisements: Emotions and empathy guide prosocial behavior. The Journal of Marketing, 58(1), 56-70.
[https://doi.org/10.1177/002224299405800105]

-
Baseman, J. G., & Koutsky, L. A. (2005). The epidemiology of human papillomavirus infections. Journal of Clinical Virology, 32(Supplement), 16-24. https://doi.org/10.1016/j.jcv.2004.12.008
[https://doi.org/10.1016/j.jcv.2004.12.008]

-
Bonafide, K. E., & Vanable, P. A. (2015). Male human papillomavirus vaccine acceptance is enhanced by a brief intervention that emphasizes both male-specific vaccine benefits and altruistic motives. Sexually Transmitted Diseases, 42(2), 76-80.
[https://doi.org/10.1097/OLQ.0000000000000226]

-
Borgstede, C. von, Andersson, M., & Hansla, A. (2014). Value-congruent information processing: The role of issue involvement and argument strength. Basic and Applied Social Psychology, 36(6), 461-477. https://doi.org/10.1080/01973533.2014.958226
[https://doi.org/10.1080/01973533.2014.958226]

-
Bosch, F. X., Lorincz, A., Muñoz, N., Meijer, C. J. L. M., & Shah, K. V. (2002). The causal relation between human papillomavirus and cervical cancer. Journal of Clinical Pathology, 55(4), 244-265.
[https://doi.org/10.1136/jcp.55.4.244]

-
Boudewyns, V., Turner, M. M., & Paquin, R. S. (2013). Shame-free guilt appeals: Testing the emotional and cognitive effects of shame and guilt appeals. Psychology & Marketing, 30(9), 811-825. https://doi.org/10.1002/mar.20647
[https://doi.org/10.1002/mar.20647]

-
Brewer, N. T., & Fazekas, K. I. (2007). Predictors of HPV vaccine acceptability: A theory-informed, systematic review. Preventive Medicine, 45(2-3), 107-114. https://doi.org/10.1016/j.ypmed.2007.05.013
[https://doi.org/10.1016/j.ypmed.2007.05.013]

-
Carpenter, C. J. (2010). A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Communication, 25(8), 661-669.
[https://doi.org/10.1080/10410236.2010.521906]

- Centers for Disease Control and Prevention. (2010). FDA licensure of bivalent human papillomavirus vaccine (HPV2, Cervarix) for use in females and updated HPV vaccination recommendations from the Advisory Committee on Immunization Practices (ACIP). Morbidity and Mortality Weekly Report, 59(20), 626-629.
- Centers for Disease Control and Prevention. (2016). HPV and men: Fact sheet. https://www.cdc.gov/std/hpv/stdfact-hpv-and-men.htm
- Centers for Disease Control and Prevention. (2019). Genital HPV infection: Fact sheet. https://www.cdc.gov/std/hpv/stdfact-hpv.htm
- Centers for Disease Control and Prevention. (2020, March 17). HPV vaccination: What everyone should know. https://www.cdc.gov/vaccines/vpd/hpv/public/index.html
-
Chon, M.-G., & Park, H. (2017). One does not fit all: Health audience segmentation and prediction of health behaviors in cancer prevention. Health Marketing Quarterly, 34(3), 202-216. https://doi.org/10.1080/07359683.2017.1346434
[https://doi.org/10.1080/07359683.2017.1346434]

-
Dearing, R. L., Stuewig, J., & Tangney, J. P. (2005). On the importance of distinguishing shame from guilt: Relations to problematic alcohol and drug use. Addictive Behaviors, 30(7), 1392-1404. https://doi.org/10.1016/j.addbeh.2005.02.002
[https://doi.org/10.1016/j.addbeh.2005.02.002]

-
Donadiki, E. M., Jiménez-García, R., Hernández-Barrera, V., Sourtzi, P., Carrasco-Garrido, P., López de Andrés, A., Jimenez-Trujillo, I., & Velonakis, E. G. (2014). Health belief model applied to non-compliance with HPV vaccine among female university students. Public Health, 128(3), 268-273. https://doi.org/10.1016/j.puhe.2013.12.004
[https://doi.org/10.1016/j.puhe.2013.12.004]

-
Ellsworth, P. C., & Smith, C. A. (1988). Shades of joy: Patterns of appraisal differentiating pleasant emotions. Cognition & Emotion, 2(4), 301-331. https://doi.org/10.1080/02699938808412702
[https://doi.org/10.1080/02699938808412702]

-
Eyler, A. A., & Vest, J. R. (2002). Environmental and policy factors related to physical activity in rural white women. Women & Health, 36(2), 111-121.
[https://doi.org/10.1300/J013v36n02_08]

-
Fallon, E. A., Wilcox, S., & Ainsworth, B. E. (2005). Correlates of self-efficacy for physical activity in African American women. Women & Health, 41(3), 47-62.
[https://doi.org/10.1300/J013v41n03_03]

-
Fallucca, A., Immordino, P., Riggio, L., Casuccio, A., Vitale, F., & Restivo, V. (2022). Acceptability of HPV vaccination in young students by exploring health belief model and health literacy. Vaccines, 10(7), Article 7. https://doi.org/10.3390/vaccines10070998
[https://doi.org/10.3390/vaccines10070998]

-
Fang, C. Y., Ma, G. X., Tan, Y., & Chi, N. (2007). A multifaceted intervention to increase cervical cancer screening among underserved Korean women. Cancer Epidemiology Biomarkers & Prevention, 16(6), 1298-1302. https://doi.org/10.1158/1055-9965.EPI-07-0091
[https://doi.org/10.1158/1055-9965.EPI-07-0091]

-
Gerend, M. A., & Barley, J. (2009). Human papillomavirus vaccine acceptability among young adult men. Sexually Transmitted Diseases, 36(1), 58-62. https://doi.org/10.1097/OLQ.0b013e31818606fc
[https://doi.org/10.1097/OLQ.0b013e31818606fc]

-
Gerend, M. A., & Shepherd, J. E. (2007). Using message framing to promote acceptance of the human papillomavirus vaccine. Health Psychology, 26(6), 745-752. https://doi.org/10.1037/0278-6133.26.6.745
[https://doi.org/10.1037/0278-6133.26.6.745]

-
Gerend, M. A., & Shepherd, J. E. (2012). Predicting human papillomavirus vaccine uptake in young adult women: Comparing the health belief model and theory of planned behavior. Annals of Behavioral Medicine, 44(2), 171-180. https://doi.org/10.1007/s12160-012-9366-5
[https://doi.org/10.1007/s12160-012-9366-5]

-
Gerend, M. A., Shepherd, J. E., & Monday, K. A. (2008). Behavioral frequency moderates the effects of message framing on HPV vaccine acceptability. Annals of Behavioral Medicine, 35(2), 221-229. https://doi.org/10.1007/s12160-008-9024-0
[https://doi.org/10.1007/s12160-008-9024-0]

-
Goldfarb, J. A., & Comber, J. D. (2022). Human papillomavirus (HPV) infection and vaccination: A cross-sectional study of college students’ knowledge, awareness, and attitudes in Villanova, PA. Vaccine: X, 10, Article 100141. https://doi.org/10.1016/j.jvacx.2022.100141
[https://doi.org/10.1016/j.jvacx.2022.100141]

-
Harrison, J. A., Mullen, P. D., & Green, L. W. (1992). A meta-analysis of studies of the health belief model with adults. Health Education Research, 7(1), 107-116.
[https://doi.org/10.1093/her/7.1.107]

-
Izard, C. E. (1977). Human emotions. New York, NY: Plenum Press.
[https://doi.org/10.1007/978-1-4899-2209-0]

-
Janz, N. K., & Becker, M. H. (1984). The health belief model: A decade later. Health Education & Behavior, 11(1), 1-47. https://doi.org/10.1177/109019818401100101
[https://doi.org/10.1177/109019818401100101]

-
Kahn, B. Z., Huang, Q., Thompson, P., Gilkey, M. B., Alton Dailey, S., & Brewer, N. T. (2023). Getting human papillomavirus vaccination back on track: A national survey. The Journal of Adolescent Health, 72(6), 950-957. https://doi.org/10.1016/j.jadohealth.2023.01.004
[https://doi.org/10.1016/j.jadohealth.2023.01.004]

-
Kim, S., & Hmielowski, J. D. (2017). The influence of self-efficacy in medical drama television programming on behaviors and emotions that promote cervical cancer prevention. American Journal of Health Behavior, 41(6), 719-727. https://doi.org/10.5993/AJHB.41.6.6
[https://doi.org/10.5993/AJHB.41.6.6]

- Kline, R. B. (2011). Principles and practice of structural equation modeling (3rd ed.). New York, NY: Guilford Press.
-
Lazarus, R. S. (1991). Emotion and adaptation. New York, NY: Oxford University Press.
[https://doi.org/10.1093/oso/9780195069945.001.0001]

-
Lee, H. Y., Lust, K., Vang, S., & Desai, J. (2018). Male undergraduates’ HPV vaccination behavior: Implications for achieving HPV-associated cancer equity. Journal of Community Health, 43(3), 459-466. https://doi.org/10.1007/s10900-018-0482-4
[https://doi.org/10.1007/s10900-018-0482-4]

-
Lee, S. Y., Hwang, H., Hawkins, R., & Pingree, S. (2008). Interplay of negative emotion and health self-efficacy on the use of health information and its outcomes. Communication Research, 35(3), 358-381. https://doi.org/10.1177/0093650208315962
[https://doi.org/10.1177/0093650208315962]

-
Macintyre, K., Rutenberg, N., Brown, L., & Karim, A. (2004). Understanding perceptions of HIV risk among adolescents in KwaZulu-Natal. AIDS and Behavior, 8(3), 237-250.
[https://doi.org/10.1023/B:AIBE.0000044072.71361.b3]

-
Markowitz, L. E., Dunne, E. F., Saraiya, M., Lawson, H. W., Chesson, H., & Unger, E. R. (2007). Quadrivalent human papillomavirus vaccine: Recommendations of the advisory committee on immunization practices (ACIP). Morbidity and Mortality Weekly Report: Recommendations and Reports, 56(RR-2), 1-23.
[https://doi.org/10.1037/e601292007-001]

-
McLendon, L., Puckett, J., Green, C., James, J., Head, K. J., Yun Lee, H., Young Pierce, J., Beasley, M., & Daniel, C. L. (2021). Factors associated with HPV vaccination initiation among United States college students. Human Vaccines & Immunotherapeutics, 17(4), 1033-1043. https://doi.org/10.1080/21645515.2020.1847583
[https://doi.org/10.1080/21645515.2020.1847583]

-
McPartland, T. S., Weaver, B. A., Lee, S.-K., & Koutsky, L. A. (2005). Men’s perceptions and knowledge of human papillomavirus (HPV) infection and cervical cancer. Journal of American College Health, 53(5), 225-230. https://doi.org/10.3200/JACH.53.5.225-230
[https://doi.org/10.3200/JACH.53.5.225-230]

-
Meites, E., Szilagyi, P. G., Chesson, H. W., Unger, E. R., Romero, J. R., & Markowitz, L. E. (2019). Human papillomavirus vaccination for adults: Updated recommendations of the advisory committee on immunization practices. Morbidity and Mortality Weekly Report, 68(32), 698-702. https://doi.org/10.15585/mmwr.mm6832a3
[https://doi.org/10.15585/mmwr.mm6832a3]

-
Montanaro, E. A., & Bryan, A. D. (2014). Comparing theory-based condom interventions: Health belief model versus theory of planned behavior. Health Psychology, 33(10), 1251.
[https://doi.org/10.1037/a0033969]

-
Nabi, R. L., & Myrick, J. G. (2019). Uplifting fear appeals: Considering the role of hope in fear-based persuasive messages. Health Communication, 34(4), 463-474. https://doi.org/10.1080/10410236.2017.1422847
[https://doi.org/10.1080/10410236.2017.1422847]

- Office of Disease Prevention and Health Promotion. (n.d.). Increase the proportion of adolescents who get recommended doses of the HPV vaccine—IID-08. https://health.gov/healthypeople/objectives-and-data/browse-objectives/vaccination/increase-proportion-adolescents-who-get-recommended-doses-hpv-vaccine-iid-08
-
Oh, K. M., Alqahtani, N., Chang, S., & Cox, C. (2023). Knowledge, beliefs, and practice regarding human papillomavirus (HPV) vaccination among American college students: Application of the health belief model. Journal of American College Health, 71(8), 2329-2338. https://doi.org/10.1080/07448481.2021.1967362
[https://doi.org/10.1080/07448481.2021.1967362]

-
Radisic, G., Chapman, J., Flight, I., & Wilson, C. (2017). Factors associated with parents’ attitudes to the HPV vaccination of their adolescent sons: A systematic review. Preventive Medicine, 95, 26-37. https://doi.org/10.1016/j.ypmed.2016.11.019
[https://doi.org/10.1016/j.ypmed.2016.11.019]

-
Rosenstock, I. M. (1974). Historical origins of the health belief model. Health Education & Behavior, 2(4), 328-335.
[https://doi.org/10.1177/109019817400200403]

-
Rosenstock, I. M., Strecher, V. J., & Becker, M. H. (1988). Social learning theory and the health belief model. Health Education & Behavior, 15(2), 175-183.
[https://doi.org/10.1177/109019818801500203]

-
Rositch, A. F., Liu, T., Chao, C., Moran, M., & Beavis, A. L. (2022). Levels of parental human papillomavirus vaccine hesitancy and their reasons for not intending to vaccinate: Insights from the 2019 national immunization survey-teen. Journal of Adolescent Health, 71(1), 39-46. https://doi.org/10.1016/j.jadohealth.2022.01.223
[https://doi.org/10.1016/j.jadohealth.2022.01.223]

-
Schofield, I., Kerr, S., & Tolson, D. (2007). An exploration of the smoking-related health beliefs of older people with chronic obstructive pulmonary disease. Journal of Clinical Nursing, 16(9), 1726-1735. https://doi.org/10.1111/j.1365-2702.2007.01701.x
[https://doi.org/10.1111/j.1365-2702.2007.01701.x]

-
Schuler, C. L., DeSousa, N. S., & Coyne-Beasley, T. (2014). Parents’ decisions about hpv vaccine for sons: The importance of protecting sons’ future female partners. Journal of Community Health, 39(5), 842-848. https://doi.org/10.1007/s10900-014-9859-1
[https://doi.org/10.1007/s10900-014-9859-1]

-
Schwarzer, R., Schuz, B., Ziegelmann, J. P., Lippke, S., Luszczynska, A., & Scholz, U. (2007). Adoption and maintenance of four health behaviors: Theory-guided longitudinal studies on dental flossing, seat belt use, dietary behavior, and physical activity. Annals of Behavioral Medicine, 33(2), 156-166. https://doi.org/10.1007/BF02879897
[https://doi.org/10.1007/BF02879897]

-
Shand, L., Burney, S., & Fletcher, J. (2010). Knowledge of cervical cancer, pap testing and the human papillomavirus among young Australian women. Health Promotion Journal of Australia, 21(3), 202-207.
[https://doi.org/10.1071/HE10202]

-
Smith, C. A., & Lazarus, R. S. (1993). Appraisal components, core relational themes, and the emotions. Cognition and Emotion, 7, 233-269.
[https://doi.org/10.1080/02699939308409189]

-
Smith, C. A., Haynes, K. N., Lazarus, R. S., & Pope, L. K. (1993). In search of the “hot” cognitions: Attributions, appraisals, and their relation to emotion. Journal of Personality and Social Psychology, 65(5), 916-929. https://doi.org/10.1037/0022-3514.65.5.916
[https://doi.org/10.1037/0022-3514.65.5.916]

-
Staggers, S. M., Brann, M., & Maki, S. M. (2012). Let’s talk about HPV: Examining college male perceptions of the HPV vaccine. Qualitative Research Reports in Communication, 13(1), 28-36. https://doi.org/10.1080/17459435.2012.719206
[https://doi.org/10.1080/17459435.2012.719206]

-
Steins, G., & Weiner, B. (1999). The influence of perceived responsibility and personality characteristics on the emotional and behavioral reactions to people with AIDS. The Journal of Social Psychology, 139(4), 487-495.
[https://doi.org/10.1080/00224549909598408]

-
Walker, T. Y., Elam-Evans, L. D., Yankey, D., Markowitz, L. E., Williams, C. L., Fredua, B., Singleton, J. A., & Stokley, S. (2019). National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 years-United States, 2018. Morbidity and Mortality Weekly Report, 68(33). https://doi.org/10.15585/mmwr.mm6833a2
[https://doi.org/10.15585/mmwr.mm6833a2]

-
Wang, X. (2023). Putting emotions in the health belief model: The role of hope and anticipated guilt on the Chinese’s intentions to get COVID-19 vaccination. Health Communication, 38(11), 2491-2500. https://doi.org/10.1080/10410236.2022.2078925
[https://doi.org/10.1080/10410236.2022.2078925]

-
Wayment, H. A., & Aronson, B. (2002). Risky sexual behavior in American white college women: The role of sex guilt and sexual abuse. Journal of Health Psychology, 7(6), 723-733. https://doi.org/10.1177/1359105302007006876
[https://doi.org/10.1177/1359105302007006876]

-
Wilson, K. L., White, A., Rosen, B. L., Chiappone, A., Pulczinski, J. C., Ory, M. G., & Smith, M. L. (2016). Factors associated with college students’ intentions to vaccinate their daughters against HPV: Protecting the next generation. Journal of Community Health, 41(5), 1078-1089. https://doi.org/10.1007/s10900-016-0192-8
[https://doi.org/10.1007/s10900-016-0192-8]

-
Wolitski, R. J., Bailey, C. J., O’Leary, A., Gomez, C. A., & Parsons, J. T. (2003). Self-perceived responsibility of HIV-seropositive men who have sex with men for preventing HIV transmission. AIDS and Behavior, 7(4), 363-372.
[https://doi.org/10.1023/B:AIBE.0000004728.73443.32]

-
Wu, T.-Y., West, B., Chen, Y.-W., & Hergert, C. (2006). Health beliefs and practices related to breast cancer screening in Filipino, Chinese and Asian-Indian women. Cancer Detection and Prevention, 30(1), 58-66. https://doi.org/10.1016/j.cdp.2005.06.013
[https://doi.org/10.1016/j.cdp.2005.06.013]

-
Xiao, X., Lee, D. K. L., Wong, R. M., & Borah, P. (2021). The impact of theory in HPV vaccination promotion research: A systematic review and meta-analysis. American Journal of Health Promotion, 35(7), 1002-1014. https://doi.org/10.1177/08901171211012524
[https://doi.org/10.1177/08901171211012524]

-
Zak-Place, J., & Stern, M. (2004). Health belief factors and dispositional optimism as predictors of STD and HIV preventive behavior. Journal of American College Health, 52(5), 229-236.
[https://doi.org/10.3200/JACH.52.5.229-236]

